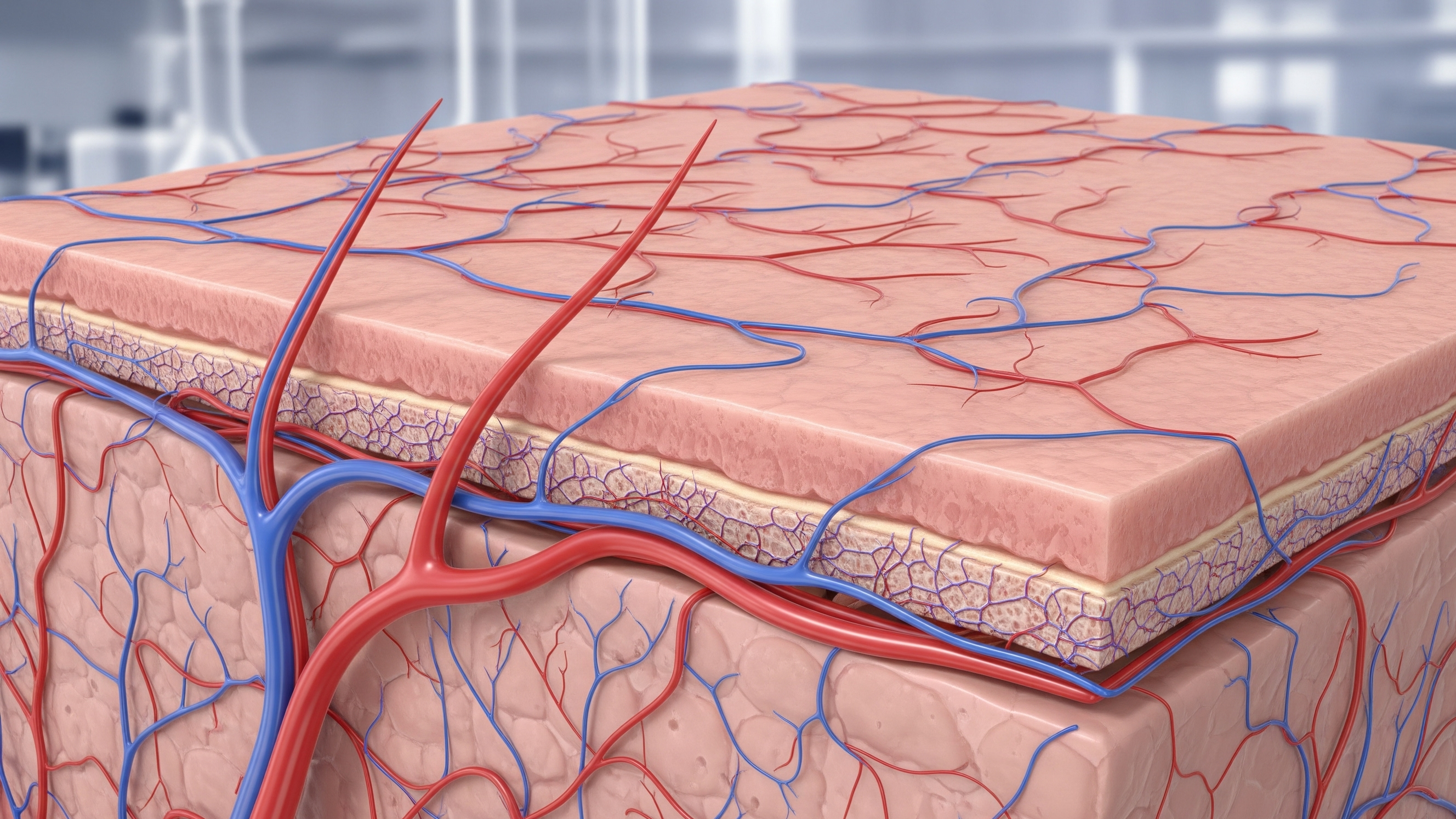
Skin is the body’s border and its promise. It keeps us intact, it repairs when we break, it carries sensation and identity.
For decades, medicine tried to replace it when it failed. We used grafts, donor tissue, synthetic sheets. They helped, but only in parts. What we could not rebuild was living skin that feeds itself, feels, and survives long term on the body.
That’s the shift here. In Brisbane, researchers at the University of Queensland’s Frazer Institute have grown a lab-made human skin that includes its own blood supply, with blood vessels and capillaries running through it, along with hair follicles, nerves, layered tissue, and immune cells (ABC News, NDTV).
The work comes out of UQ’s Frazer Institute in Queensland under Dr Abbas Shafiee and Professor Kiarash Khosrotehrani.
Reports identify the team and frame it as six years of development, from concept to a functional model that behaves like real human skin in the lab (Sarawak Tribune).
What actually changed technically
This wasn’t just “more cells.” The researchers took human skin cells, reprogrammed them into stem cells, and grew miniature skin organoids in dishes.
They then engineered tiny blood vessels from the same stem cells and integrated them into the developing tissue.
The result is a vascularized skin construct that matures with layers, appendage patterning, pigmentation, and innervation, all missing from previous models.
Non-vascular skin equivalents dry out, fail to integrate, and often can’t survive once grafted.
Adding a blood supply changes the biology. It supports nutrient flow, waste removal, and immune signaling, which means the tissue can be studied like skin and, in time, could be prepared to connect with a patient’s circulation (NDTV, Medical Dialogues).
What It Can Do Today and What It Can’t (Yet)
The immediate value is disease modeling and drug testing in a system that behaves like human skin. Early targets include psoriasis, atopic dermatitis, and scleroderma.
With hair follicles, nerves, immune cells, and vasculature in place, researchers can watch how inflammation spreads, how immune cells migrate, and how candidate therapies perform in a realistic environment.
It is not ready for clinical grafting on patients.
The researchers themselves say graft use is “down the track,” after safety testing, vascular integration studies, and regulatory steps. So the promise is real, but the timeline is science, not hype (ABC, NDTV).
Why Queensland, why now
Queensland has one of the world’s highest skin cancer rates, and more than 3,600 Queenslanders are diagnosed with melanoma each year.

A robust, human-like skin model could accelerate prevention science, early detection studies, and reconstructive research for burns and surgical defects (Health and Me, OnlyMyHealth).
For now, the consensus across reports is aligned: this is a world-first, lab-grown human skin with its own blood supply, built by the UQ team, validated by multiple outlets, and positioned first for research, with clinical applications to come.